Desperate for constipation relief? Before you reach for harsh laxatives, understand why they often fail and can worsen IBS-C. This science-backed emergency plan uses gentle, proven methods to calm your nervous system and safely restart digestion.
If you’re reading this, you’re likely in a state of discomfort, anxiety, and even panic. The urge to grab the strongest laxative on the shelf is overwhelming. You want it to work, and you want it to work now.
That instinct is completely understandable. But if you have IBS-C, that approach can often backfire, leading to more pain and a worsening cycle. This guide offers you a different path—one that is both gentle and grounded in physiology and clinical research—to help you through this acute flare-up safely and effectively.
Why Your Go-To Remedies Fail (And Can Make Things Worse)
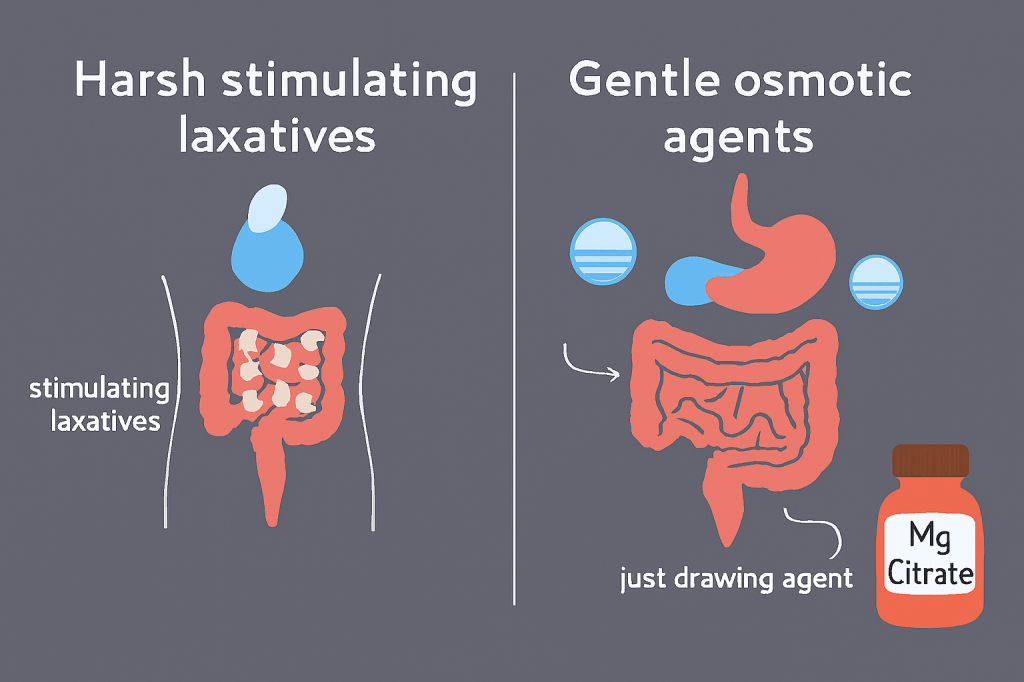
When you’re desperate, you might reach for stimulant laxatives like senna or bisacodyl. They work by aggressively forcing your colon to contract. Here’s the problem for IBS-C:
- They Ignore the Root Cause: For many with IBS-C, constipation is not just a lazy colon; it’s often a nervous system in a protective “freeze” state (dorsal vagal shutdown). A 2021 review in The Lancet Gastroenterology & Hepatology notes that stress and anxiety are key amplifiers of IBS symptoms, directly affecting gut motility. Forcing a clenched system to contract can be intensely painful.
- They Can Worsen the Cycle: Stimulants can cause cramping, dehydration, and electrolyte loss. With regular use, your colon can become dependent on them, a condition sometimes referred to as “lazy bowel syndrome” or cathartic colon, making natural function even harder in the long run.
So, what’s the alternative when you’re truly stuck?
The Science-Backed, “Safety-First” Emergency Plan
This plan works with your body’s physiology, not against it. The core principle is simple: Signal “safety” to your nervous system first, then use gentle, osmotic methods to encourage movement.
Step 1: The Immediate Nervous System Reset (First 30 Minutes)
Before you ingest anything, you must lower the alarm signal. Anxiety directly inhibits the vagus nerve, your main “rest-and-digest” nerve.
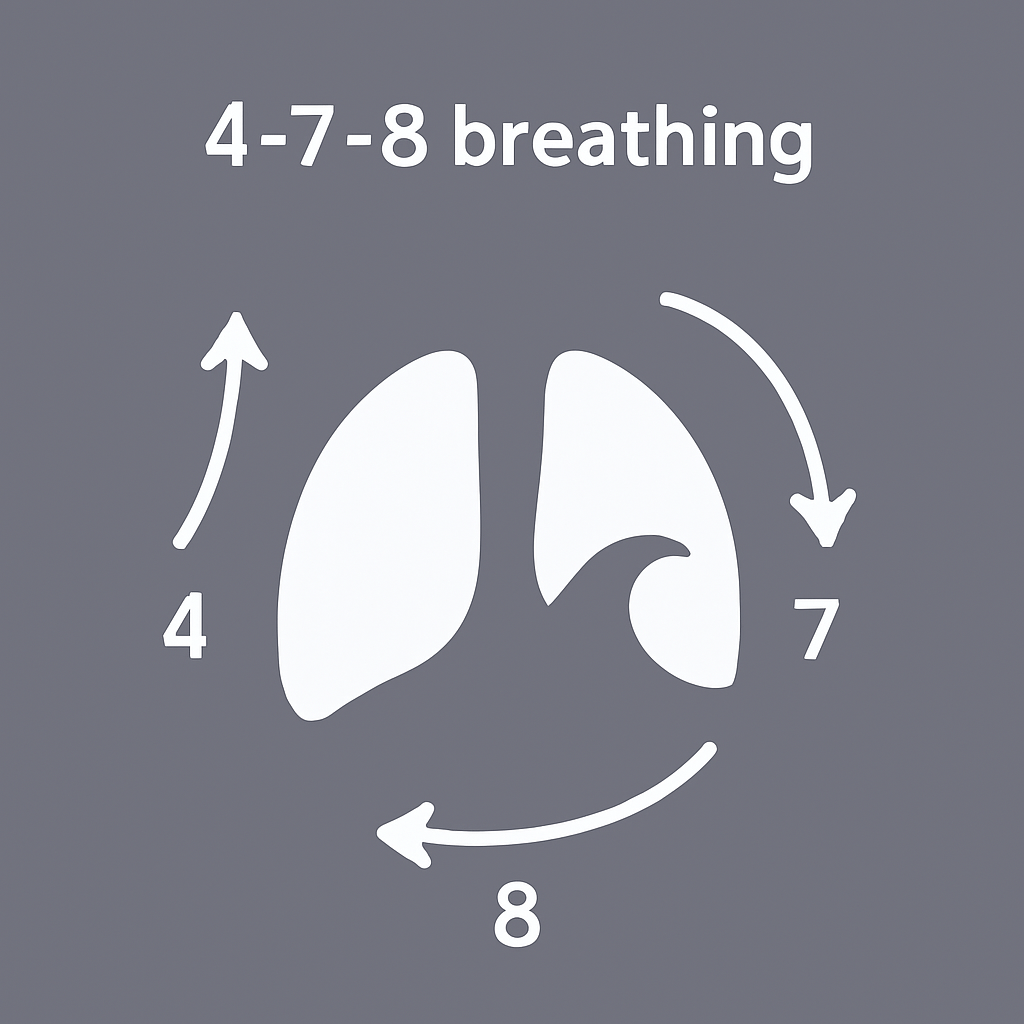
- The Evidence-Based Practice: 4-7-8 Breathing. Research, including studies published in Frontiers in Human Neuroscience, shows that prolonged exhales (like the 4-7-8 technique) increase vagal tone, slowing heart rate and promoting a state of calm.
- Your Action: Sit quietly. Inhale through your nose for 4 seconds, hold for 7, exhale through your mouth for 8. Repeat for 5 minutes. This is not a relaxation exercise; it’s a physiological intervention to dial down the “freeze” response that is locking your gut.
Step 2: The Gentle, Physiologic Nudge (Next 1-2 Hours)
Now, we use the most trusted first-line recommendation from gastroenterologists for acute episodes: osmotic agents.
- The Science: Osmotics like magnesium citrate or polyethylene glycol (PEG 3350) work by drawing water into the colon from surrounding tissues. This softens the stool and gently distends the colon wall, which naturally triggers peristalsis (the wave-like contractions to move things along). They are not stimulants; they are hydrators.
- Your Action (Consult Your Doctor First):
- Magnesium Citrate: A dose of 200-400mg with a large glass of warm water is a common starting point. It provides the dual benefit of osmotic action and magnesium, which is a natural muscle relaxant. For a complete guide to choosing the right type and dose for IBS-C, see our detailed article: Magnesium for Constipation & IBS-C: Citrate vs. Glycinate.
- Electrolyte Support: Drink warm water with lemon and a pinch of sea salt. Proper hydration and electrolytes are critical for all muscle function, including your colon’s.
Step 3: Supportive Physical Signals
Combine the above with gentle, supportive movement.
- Abdominal Massage: A clinical practice guideline published in Gastroenterology & Hepatology acknowledges abdominal massage as a beneficial complementary therapy for constipation, helping to reduce severity and stimulate activity.
- Your Action: Using the palm of your hand, apply firm but gentle pressure and massage in a clockwise circle around your navel, following the path of your colon.
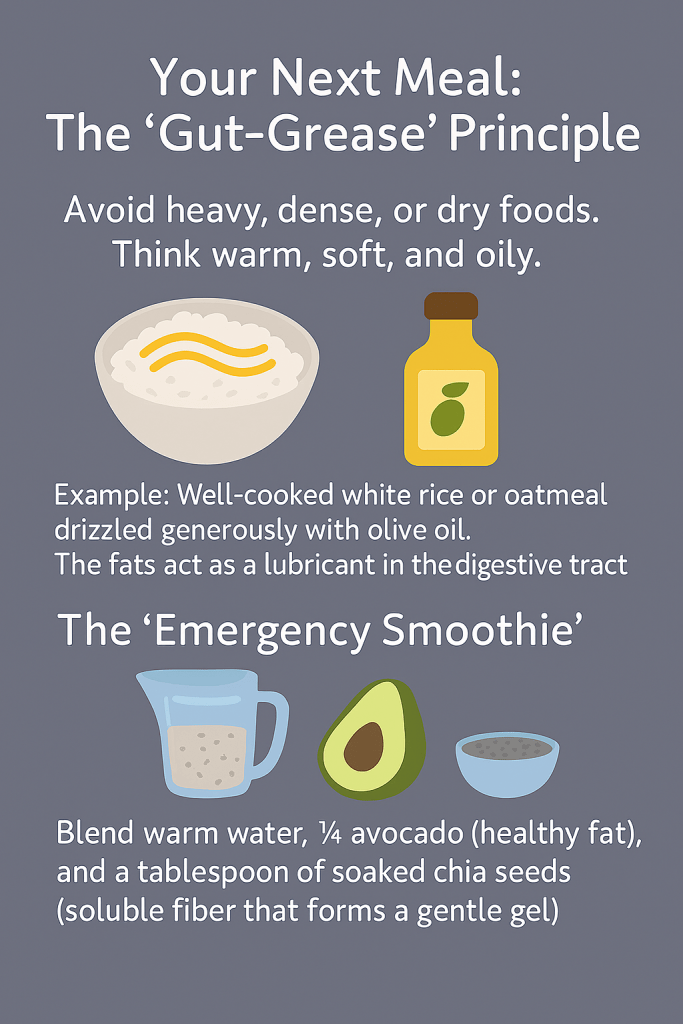
Your Next Meal: The “Gut-Grease” Principle
Avoid heavy, dense, or dry foods. Think warm, soft, and oily.
- Example: Well-cooked white rice or oatmeal drizzled generously with olive oil. The fats act as a lubricant in the digestive tract.
- The “Emergency Smoothie”: Blend warm water, ¼ avocado (healthy fat), and a tablespoon of soaked chia seeds (soluble fiber that forms a gentle gel).
The Critical Mindset Shift: From Attack to Alliance
This flare-up is a signal. If you find that you repeatedly end up here despite various diets and supplements, it’s strong evidence that the issue is not just in your gut, but in your gut-brain axis.
Chronically stressed nervous systems keep the gut in a guarded state. The solution isn’t a stronger laxative; it’s a calmer foundation. To understand this core connection better, start with our guide: IBS-C 101: When Your Gut is a Nervous System Alarm.
When laxatives, fibers, and diets have all failed you, the real problem isn’t your gut—it’s adaptation. You’ve been trying to force a system that feels unsafe to function.
It’s time to learn its language. My free 7-Day Vagus-Vital Starter Guide teaches you how to build that foundation of nervous system safety daily, so these desperate emergencies become a thing of the past.
Disclaimer: This post shares insights from my 15-year journey with IBS-C and is for educational purposes only. It is not medical advice. Please consult your doctor before making any changes to your diet, supplements, or health routine.

Leave a comment