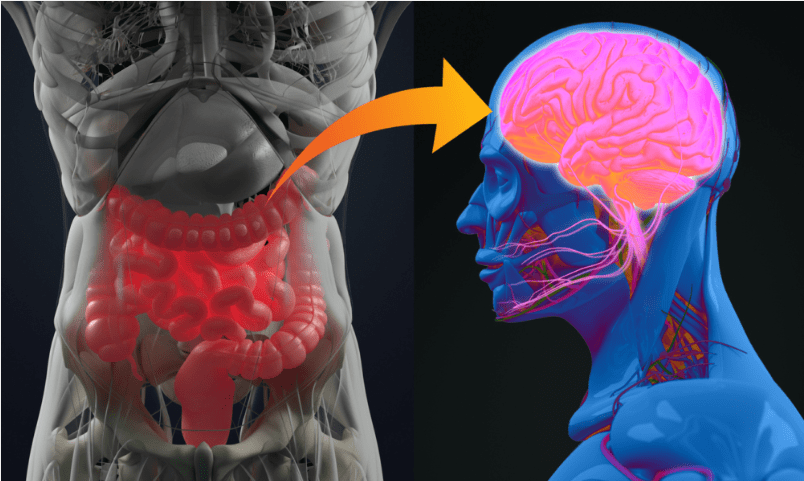
That bloated, sluggish, “stuck” feeling in your gut often comes with a similar feeling in your mind: brain fog, low mood, and a background hum of anxiety. If you’re searching for answers to the constipation anxiety loop, understand that this isn’t just a coincidence – it’s biology.
Emerging research confirms a powerful two-way street between your digestive rhythm and your mental state. If you’re constipated, you’re not just physically backed up; your brain is receiving stress signals that can fuel worry and fatigue. This article breaks down the science of this cycle and gives you a practical 4-step protocol to break it.
The Gut-Brain Axis in Anxiety: More Than Just a Feeling
We often think of anxiety as starting with a worry. But what if it starts with a stalled gut? The gut-brain axis is a constant, bi-directional conversation via the vagus nerve, hormones, and immune messengers. When your gut motility slows (constipation), it doesn’t just cause local discomfort; it changes the entire conversation, sending signals of dysregulation and distress to your brain.
The Science of the Constipation-Anxiety Loop: A Vicious Cycle
Constipation from a gut-brain perspective is a sign of a deeper communication breakdown. Here’s what’s really happening:
- The Vagus Nerve Goes Silent: Your vagus nerve is the main communication highway for promoting digestion. Chronic stress suppresses it, creating a cycle: stress → low vagal tone → constipation → more stress signals. I explore how to activate it directly in my post on The Vagus Nerve & Bowel Movements.
- The Bacterial Balance Shifts: A slow-moving gut allows bacteria to overgrow, producing inflammatory metabolites that can affect mood.
- Inflammation Travels to Your Brain: Constipation and dysbiosis can weaken the gut lining. This allows inflammatory molecules to escape, travel to the brain, and disrupt neurotransmitter function, fueling anxiety (as noted in research like a 2020 Nature Reviews Immunology article).
- The Serotonin Connection Gets Blocked: Your gut produces most of your body’s serotonin, crucial for both mood and gut motility. Constipation and inflammation impair this, trapping you in the loop.
The 4-Step Gut-Brain Protocol to Break the Cycle
Healing requires addressing both ends of the axis: calming the mind to help the gut, and supporting the gut to calm the mind.
Step 1: Activate Your Vagus Nerve (Send “Safety” Signals)
- Deep, Diaphragmatic Breathing: 5 minutes before meals to prime your gut for digestion.
- The “Physiological Sigh”: Inhale deeply, take one more sip of air, exhale slowly. Do for 30 seconds to quickly reduce stress.
Step 2: Nourish with Foundational Nutrients
- Magnesium Glycinate (200-400mg): Draws water into the intestines, relaxes muscles, and supports nerve function. Take with dinner. (For a deep dive on choosing the right type, see my guide on Magnesium for IBS-C: Citrate vs. Glycinate).
- Vitamin C (500-1000mg): Has an osmotic effect in the colon to soften stool and acts as an anti-inflammatory.
- High-Quality Omega-3s (EPA/DHA): Essential for reducing the systemic inflammation that disrupts gut-brain signaling, with studies linking it to reduced anxiety.
Step 3: Rebuild with Smart Fiber
- Start Slow with Soluble Fiber: Like ground flaxseed or psyllium husk. It feeds beneficial bacteria gently without excessive gas.
Step 4: Master the Mind-Gut Rhythm
- Honor Hunger Cues: Eat in a calm state, not when stressed.
- Establish Routine: Consistent meal and bathroom times help regulate your gut. A structured approach can help; see my IBS-C Morning Routine for ideas.
- Move Your Body: Gentle daily walks improve motility and reduce anxiety.
Key Mind-Body Takeaways
Constipation is more than a physical inconvenience; it’s a signal that the gut-brain dialogue is distressed. You can’t simply “think” your way out of constipation, nor “supplement” your way out of the anxiety it fuels.
The solution lies in interrupting the constipation-anxiety loop at both ends: using nervous system regulation (vagus nerve work) to send safety signals downward, and using foundational nutrition to heal the communication pathways upward.
Ready to apply this? Get my free ‘7-Day Guide to Calming the Gut-Brain Loop’, which turns these steps into a daily, actionable plan with checklists and deeper insights.That bloated, sluggish, “stuck” feeling in your gut often comes with a similar feeling in your mind: brain fog, low mood, and a background hum of anxiety. If you’re searching for answers to the constipation anxiety loop, understand that this isn’t just a coincidence—it’s biology. Emerging research confirms a powerful two-way street between your digestive rhythm and your mental state. If you’re constipated, you’re not just physically backed up; your brain is receiving stress signals that can fuel worry and fatigue. This article breaks down the science of this cycle and gives you a practical 4-step protocol to break it.
The Gut-Brain Axis in Anxiety: More Than Just a Feeling
We often think of anxiety as starting with a worry. But what if it starts with a stalled gut? The gut-brain axis is a constant, bi-directional conversation via the vagus nerve, hormones, and immune messengers. When your gut motility slows (constipation), it doesn’t just cause local discomfort; it changes the entire conversation, sending signals of dysregulation and distress to your brain.
The Science of the Constipation-Anxiety Loop: A Vicious Cycle
Constipation from a gut-brain perspective is a sign of a deeper communication breakdown. Here’s what’s really happening:
- The Vagus Nerve Goes Silent: Your vagus nerve is the main communication highway for promoting digestion. Chronic stress suppresses it, creating a cycle: stress → low vagal tone → constipation → more stress signals. I explore how to activate it directly in my post on The Vagus Nerve & Bowel Movements.
- The Bacterial Balance Shifts: A slow-moving gut allows bacteria to overgrow, producing inflammatory metabolites that can affect mood.
- Inflammation Travels to Your Brain: Constipation and dysbiosis can weaken the gut lining. This allows inflammatory molecules to escape, travel to the brain, and disrupt neurotransmitter function, fueling anxiety (as noted in research like a 2020 Nature Reviews Immunology article).
- The Serotonin Connection Gets Blocked: Your gut produces most of your body’s serotonin, crucial for both mood and gut motility. Constipation and inflammation impair this, trapping you in the loop.
The 4-Step Gut-Brain Protocol to Break the Cycle

Healing requires addressing both ends of the axis: calming the mind to help the gut, and supporting the gut to calm the mind.
Step 1: Activate Your Vagus Nerve (Send “Safety” Signals)
- Deep, Diaphragmatic Breathing: 5 minutes before meals to prime your gut for digestion.
- The “Physiological Sigh”: Inhale deeply, take one more sip of air, exhale slowly. Do for 30 seconds to quickly reduce stress.
Step 2: Nourish with Foundational Nutrients
- Magnesium Glycinate (200-400mg): Draws water into the intestines, relaxes muscles, and supports nerve function. Take with dinner. (For a deep dive on choosing the right type, see my guide on Magnesium for IBS-C: Citrate vs. Glycinate).
- Vitamin C (500-1000mg): Has an osmotic effect in the colon to soften stool and acts as an anti-inflammatory.
- High-Quality Omega-3s (EPA/DHA): Essential for reducing the systemic inflammation that disrupts gut-brain signaling, with studies linking it to reduced anxiety.
Step 3: Rebuild with Smart Fiber
- Start Slow with Soluble Fiber: Like ground flaxseed or psyllium husk. It feeds beneficial bacteria gently without excessive gas.
Step 4: Master the Mind-Gut Rhythm
- Honor Hunger Cues: Eat in a calm state, not when stressed.
- Establish Routine: Consistent meal and bathroom times help regulate your gut. A structured approach can help; see my IBS-C Morning Routine for ideas.
- Move Your Body: Gentle daily walks improve motility and reduce anxiety.
Key Mind-Body Takeaways
Constipation is more than a physical inconvenience; it’s a signal that the gut-brain dialogue is distressed. You can’t simply “think” your way out of constipation, nor “supplement” your way out of the anxiety it fuels.
The solution lies in interrupting the constipation-anxiety loop at both ends: using nervous system regulation (vagus nerve work) to send safety signals downward, and using foundational nutrition to heal the communication pathways upward.
Your Next Step:
If you’re ready to move from symptom management to nervous-system healing, download my free 7-Day Vagus-Vital Starter Guide. It’s designed for those with anxiety-related IBS-C (constipation) who want a clear, gentle path to digestive ease.
👉 Enter your email below to get instant free-guide access:
Disclaimer: This post shares insights from my 15-year journey with IBS-C and is for educational purposes only. It is not medical advice. Please consult your doctor before making any changes to your diet, supplements, or health routine.

Leave a comment